SAI
Introduction
Shoulder subacromial impingement syndrome results in pain, and sometimes weakness and loss of movement of the shoulder with overhead activities and activities working away from the side of the body (reaching).
The subacromial bursa and rotator cuff muscle tendons lie within the subacromial space on top of the shoulder. Subacromial impingement refers to a condition when these tendons are caught when the arm is raised from the side of the body towards and above shoulder height. In the majority of cases subacromial impingement is due to postural, flexibility and muscle imbalances.
Diagnosis
Shoulder impingement is a clinical diagnosis. The pain is usually felt down the side of the shoulder and can extend towards but not beyond the elbow. Pain comes on when the arm is lifted away from the side of the body (painful arc), over head and behind the back. With time, the shoulder may become increasingly stiff with reduced range of movement due to pain.
X-rays or other scans are not routinely required but may be requested to rule out other conditions or prior to considering a steroid injection if there is concern regarding the possibility of a rotator cuff tendon tear.
Management without surgery
Most cases of shoulder impingement can be managed successfully with activity modification, pain killers, physiotherapy and injections. Physiotherapy is the mainstay of treatment and all the other modalities, including injections, are simply to enable you to be pain free enough to carry out your exercise regime to achieve your goals. Follow the links below for more help!
Getting the most from your exercise
Management with surgery
If physiotherapy fails to resolve symptoms for at least six months if not longer, you may be offered surgical treatment. The most common procedure performed for this condition is named, “subacromial decompression”. The subacromial space is cleared of any inflammatory tissue, a ligament that holds the space tight is released and a small amount of bone is shaved away to flatten the bone above the space that might catch the tendons below.
The operation is normally performed under general anaesthetic and a nerve block to provide good pain relief after the surgery. It can also be performed with you completely awake just with a nerve block. This means you can watch the surgery taking place on the screen, you won’t feel drowsy or sick afterwards and you’ll be discharged very quickly after the customary tea and toast! Let us know if you would like to consider awake surgery as only certain lists are set up to provide this service.
After Surgery
Your arm will be placed into a collar and cuff sling and the physiotherapists will tell you what you should do with your shoulder. The surgery is performed as a day case procedure, unless it is not safe to do so. It is common to have swelling because of the surgery and the wounds are stitched. At 10 days following surgery, the stitches and dressings are removed at your GP practise. There really are no restrictions on your range of movement postop but pain will be the limiting factor. Most people end up removing the sling after a couple of days.
Complications
Common risks include bleeding, infection, pain and stiffness in the shoulder.
Specific risks with this operation are
Failure to get rid of your pain (10-15%)
Nerve injury (<0.1%)
Further surgery required if fails to work
Results
85-90% of those undergoing this surgery for impingement get better by around 6-9 months following surgery.
ACJ
Cuff Tear
Shoulder Instability
aTSR
rTSR
Shoulder Problems
Common Causes of Shoulder Problems and Pain
At Shoulder2Wrist, we understand that shoulder pain can significantly impact your daily life. There are various reasons why you might be experiencing discomfort:
Shoulder / Subacromial Impingement: This painful condition, while not fully understood, is quite common.
Frozen Shoulder: A condition that restricts normal joint movement and leads to persistent pain.
Rotator Cuff Tears: The rotator cuff, a crucial group of muscles and tendons around the shoulder joint, may be damaged, leading to instability.
Shoulder Instability: Whether following an injury or not, an unstable shoulder can cause significant distress.
Acromioclavicular Joint Issues: Conditions like osteoarthritis or instability can affect the joint on top of the shoulder.
Arthritis in the Shoulder Joint: A condition that results in inflammation and pain.
Fractured Bones: The humerus or collarbone (clavicle) may be broken, leading to considerable discomfort.
Seeking Relief and Treatment
Shoulder pain shouldn't hold you back from living life to the fullest. There are steps you can take to manage the discomfort on your own, such as using painkillers and ice packs to reduce inflammation.
However, if your symptoms persist and affect your quality of life, it's time to consider professional treatment options:
Physiotherapy: Targeted exercises and therapies can help improve shoulder function and reduce pain.
Injections: Our expert team may recommend injections, including steroids and other appropriate medications, to alleviate discomfort.
Surgical Intervention: In some cases, surgery may be necessary to address underlying issues and restore shoulder stability.
At Shoulder2Wrist, we are dedicated to providing comprehensive care and personalised treatment plans to help you regain shoulder health and function. Don't let shoulder pain hold you back - take the first step towards a pain-free life by scheduling a consultation with our experienced team today.
Shoulder Impingement (subacromial impingement)
Introduction
Shoulder subacromial impingement syndrome results in pain, and sometimes weakness and loss of movement of the shoulder with overhead activities and activities working away from the side of the body (reaching).
The subacromial bursa and rotator cuff muscle tendons lie within the subacromial space on top of the shoulder. Subacromial impingement refers to a condition when these tendons are caught when the arm is raised from the side of the body towards and above shoulder height. In the majority of cases subacromial impingement is due to postural, flexibility and muscle imbalances.
Diagnosis
Shoulder impingement is a clinical diagnosis. The pain is usually felt down the side of the shoulder and can extend towards but not beyond the elbow. Pain comes on when the arm is lifted away from the side of the body (painful arc), over head and behind the back. With time, the shoulder may become increasingly stiff with reduced range of movement due to pain.
X-rays or other scans are not routinely required but may be requested to rule out other conditions or prior to considering a steroid injection if there is concern regarding the possibility of a rotator cuff tendon tear.
Management without surgery
Most cases of shoulder impingement can be managed successfully with activity modification, pain killers, physiotherapy and injections. Physiotherapy is the mainstay of treatment and all the other modalities, including injections, are simply to enable you to be pain free enough to carry out your exercise regime to achieve your goals. Follow the links below for more help!
Getting the most from your exercise
Management with surgery
If physiotherapy fails to resolve symptoms for at least six months if not longer, you may be offered surgical treatment. The most common procedure performed for this condition is named, “subacromial decompression”. The subacromial space is cleared of any inflammatory tissue, a ligament that holds the space tight is released and a small amount of bone is shaved away to flatten the bone above the space that might catch the tendons below.
The operation is normally performed under general anaesthetic and a nerve block to provide good pain relief after the surgery. It can also be performed with you completely awake just with a nerve block. This means you can watch the surgery taking place on the screen, you won’t feel drowsy or sick afterwards and you’ll be discharged very quickly after the customary tea and toast! Let us know if you would like to consider awake surgery as only certain lists are set up to provide this service.
After Surgery
Your arm will be placed into a collar and cuff sling and the physiotherapists will tell you what you should do with your shoulder. The surgery is performed as a day case procedure, unless it is not safe to do so. It is common to have swelling because of the surgery and the wounds are stitched. At 10 days following surgery, the stitches and dressings are removed at your GP practise. There really are no restrictions on your range of movement postop but pain will be the limiting factor. Most people end up removing the sling after a couple of days.
Complications
Common risks include bleeding, infection, pain and stiffness in the shoulder.
Specific risks with this operation are
Failure to get rid of your pain (10-15%)
Nerve injury (<0.1%)
Further surgery required if fails to work
Results
85-90% of those undergoing this surgery for impingement get better by around 6-9 months following surgery.
The Acromioclavicular Joint (ACJ)
Introduction
The ACJ is the junction of the clavicle with the shoulder blade. It is a very strong and stiff joint that essentially connects your arm to your body via attachments to the shoulder blade, clavicle and sternum. There are a few conditions that exist in the ACJ, but they usually cause one of two symptoms; pain or instability or both. Pain in the ACJ without proceeding injury tends to due to degenerative or inflammatory change (arthritis). Instability/dislocation is usually secondary to a significant force/injury to the point of the shoulder.
Diagnosis
Shoulder impingement is a clinical diagnosis. The pain is usually felt down the side of the shoulder and can extend towards but not beyond the elbow. Pain comes on when the arm is lifted away from the side of the body (painful arc), over head and behind the back. With time, the shoulder may become increasingly stiff with reduced range of movement due to pain.
X-rays are important in the diagnosis and will be taken. An ultrasound is useful and will be arranged if we suspect other conditions affecting the shoulder such as subacromial impingement, or if we are carrying out a guided injection into the ACJ.
Management without surgery
ACJ arthritis can be treated successfully with activity modification, pain killers and injections. Physiotherapy is of limited value in true mechanical ACJ pain as excessive stretching or strengthening tends to exacerbate the pain. It can however be useful to maintain the shoulder range of movement so that doesn’t become stiff. Injections with steroid, normally offered under ultrasound guidance work well to control true isolated ACJ pain. If they work well then that is also normally a sign that you would do well with surgery, so that in the future if injections lose their effect, you know surgery is an option for you.
Management with surgery
If the diagnosis is clear and you either fail non-operative treatment or decide that you wish to go along the surgical route, the procedure performed is an ACJ excision. Through small incisions (key-hole surgery), the joint visualised through a small camera. The end of the clavicle is excised so that with full range of movement on table there is no contact between any of the bone that remains in the joint.
The operation is normally performed under general anaesthetic and a nerve block to provide good pain relief after the surgery. It can also be performed with you completely awake just with a nerve block. This means you can watch the surgery taking place on the screen, you won’t feel drowsy or sick afterwards and you’ll be discharged very quickly after the customary tea and toast! Let us know if you would like to consider awake surgery as only certain lists are set up to provide this service.
After Surgery
Your arm will be placed into a collar and cuff sling and the physiotherapists will tell you what you should do with your shoulder. The surgery is performed as a day case procedure, unless it is not safe to do so. It is common to have swelling because of the surgery and the wounds are stitched. At 10 days following surgery, the stitches and dressings are removed at your GP practise. There really are no restrictions on your range of movement postop but pain will be the limiting factor. ACJ surgery can be quite sore and patients should be aware of this soreness which can last up to 3 months following surgery. That said the pain can be worked through and shouldn’t limit your progression with physiotherapy.
Complications
Common risks include bleeding, infection, pain and stiffness in the shoulder.
Specific risks with this operation are
Failure to get rid of your pain (10-15%)
Nerve injury (<0.1%)
Further surgery required if fails to work
Results
90% of those undergoing this surgery for ACJ pain will get better by around 3-6 months following surgery.
Rotator Cuff Tears
Introduction
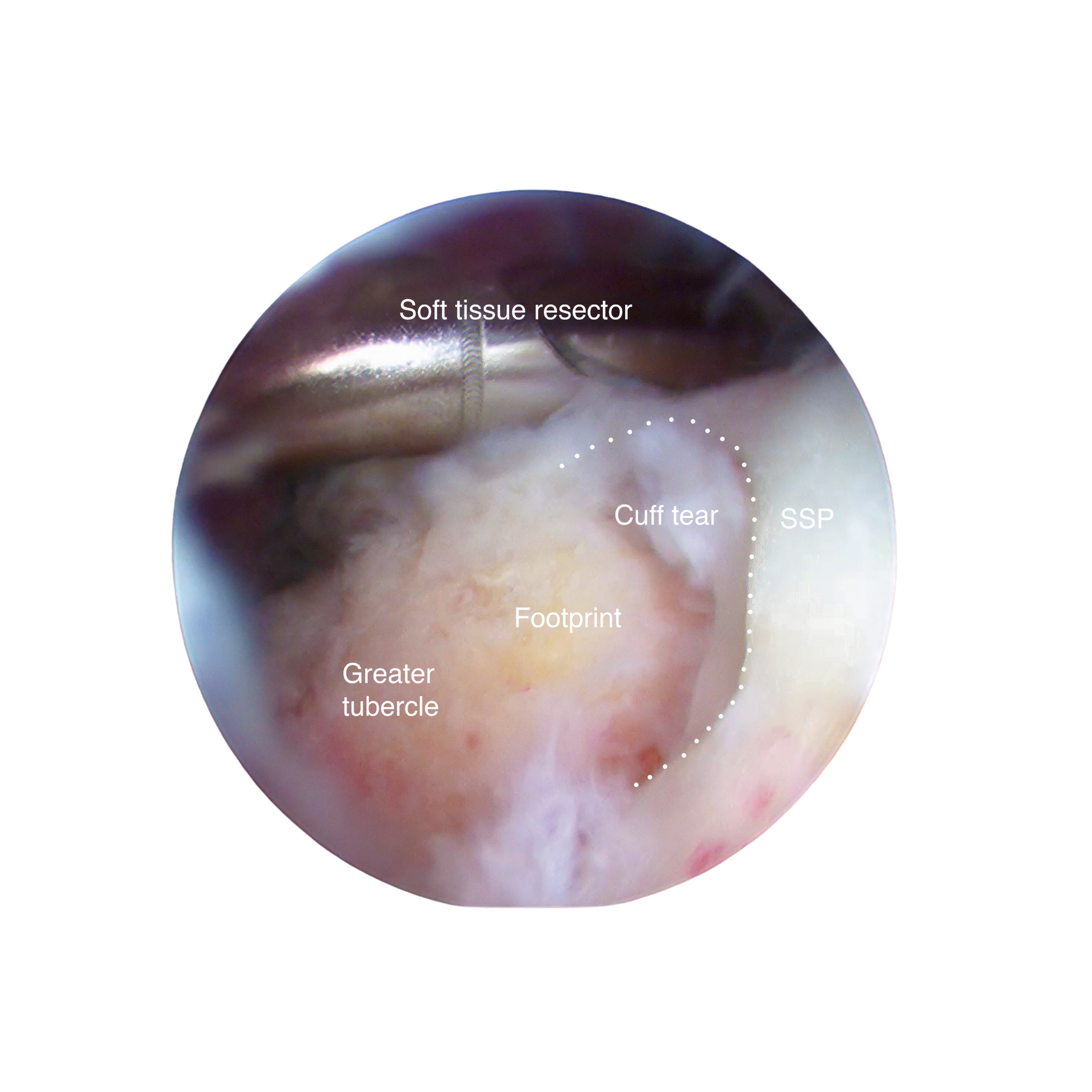
The rotator cuff tendons are four tendons that are responsible for elevation and rotation of the shoulder. They surround the ball of the ball-and-socket joint at the front (subscapularis), the top (supraspinatus) and the back (infraspinatus & teres minor). The most common location of a tear is in the top within the supraspinatus. As the tear gets bigger it extends towards the front or the back into the other tendons.
Diagnosis
New rotator cuff tears as a result of an injury often present with the same clinical picture; pain and weakness. Shoulder impingement is a clinical diagnosis. The pain is usually felt down the side of the shoulder and can extend towards but not beyond the elbow. Pain comes on when the arm is lifted away from the side of the body (painful arc), over head and behind the back. With time, the shoulder may become increasingly stiff with reduced range of movement due to pain.
X-rays or other scans are not routinely required but may be requested to rule out other conditions or prior to considering a steroid injection if there is concern regarding the possibility of a rotator cuff tendon tear.
Management without surgery
Most rotator cuff tears are degenerative and small and can be managed very successfully with activity modification, pain killers, physiotherapy and injections. Physiotherapy is the mainstay of treatment to strengthen the remaining tendons around the shoulder and improve the control of your shoulder. The other modalities, including injections, are simply to enable you to be pain free enough to carry out your exercise regime to achieve your goals.
Management with surgery
Some rotator cuff tears are acute (new tears due to an injury) or larger. Acute tears are normally offered surgery and the outcome is often better the sooner they are repaired. In addition, larger degenerative or longstanding tears may not improve clinically with physiotherapy and may require surgery. The most common procedure performed for this condition is named, “arthroscopic rotator cuff repair”. Through keyhole surgery, the tendon is cleared to healthy edges and the bone prepared to receive the tendon which is attached firmly to the bone with anchors. Occasionally, the tendon quality is poor requiring the addition of a patch of tissue to strengthen the repair, (GRAFTJACKET).
The operation is normally performed under general anaesthetic and a nerve block to provide good pain relief after the surgery. It can also be performed with you completely awake just with a nerve block. This means you can watch the surgery taking place on the screen, you won’t feel drowsy or sick afterwards and you’ll be discharged very quickly after the customary tea and toast! Let us know if you would like to consider awake surgery as only certain lists are set up to provide this service.
After Surgery
The surgery is performed as a day case procedure, unless it is not safe to do so. It is common to have swelling because of the surgery and the wounds are stitched. Your arm will be placed into a shoulder immobiliser sling and the physiotherapists will tell you what you are allowed to do with your shoulder. At 10 days following surgery, the stitches and dressings are removed at your GP practise. Physiotherapy will guide your rehabilitation and let you know when your sling can be removed; usually between 3 and 6 weeks following surgery depending on how big the tear was and how strong the repair was.
Complications
Risks include bleeding, infection, pain and stiffness in the shoulder.
Specific risks with this operation are
Failure to get rid of your pain (10-15%)
Nerve injury (<0.1%)
Further surgery required if fails to work
Results
85-90% of those undergoing rotator cuff repair will be significantly improved by 3 months following surgery and will continue to improve thereafter.
Shoulder Stabilisation for Dislocation
Introduction
Shoulder stabilisation is a procedure intended to prevent further dislocations to your shoulder thereby preventing further damage to the joint.
The Operation
You will usually be admitted on the day of surgery. The surgery will usually take place under general anaesthetic (asleep) with a nerve block for pain relief afterwards. The surgery takes between 30 and 90 minutes depending on whether you are having a key-hole (arthroscopic) stabilisation or an open operation.
Arthroscopic stabilisation
During this operation we have a full look around the shoulder to diagnose the problem. Often there is damage at the front of the joint where your shoulder has previously been coming out of joint. In these cases we free up the scarring and repair the damaged structures (often capsule) back to the socket (glenoid) where is was torn off from. There a small chance that you either don’t have anything to repair back on to the socket or there is significant bone loss within the shoulder such that we can predict the operation will fail if carried out. In these cases you may require an open operation to prevent your shoulder from dislocation or a longer period of physiotherapy to balance your shoulder properly.
Some units around the UK are performing keyhole shoulder surgery with a nerve block ONLY and the patient awake meaning they can watch the surgery taking place on a TV monitor. We are currently in discussion within our unit whether this is a possibility – the obvious benefit is that you do not feel drowsy or sick afterwards and can be discharged very quickly.
Open stabilisation (Latarjet procedure or Sheffield Bone Block procedure)
Sometimes repeated dislocations have damaged the front of the shoulder socket and the back of the ball, leading to significant bone loss. The effect of this that as the shoulder is moved into certain positions the bone defects may touch each other dislocating the shoulder. The aim of open surgery is to address the bone loss at the front of the socket to prevent this. This can be done in one of two ways:
In the Latarjet procedure, we use a piece of bone from the shoulder blade called the coracoid which is attached to the front of the shoulder along with a tendon that attaches to it. This restores the bone and the tendon acts as a sling around the shoulder to prevent dislocation. In these cases, one can expect a slight loss (probably not noticeable to you) of external rotation of the shoulder. It is however a reliable procedure with good results in the literature.
In the Sheffield Bone Block procedure (developed by Mr David Potter), half the coracoid is used as the graft without the tendon attached. This restores the bone loss well and because the tendon is left attached to its original location and not moved, full range of movement including the extremes of external rotation can be expected (good for throwing athletes). It is a relatively new procedure, but the early results are hugely promising.
After Surgery
You will be placed into a shoulder immobilising sling after the surgery and the physiotherapists will tell you what you can and can’t do with your shoulder. Most people are discharged the same day following surgery, unless it is not safe to do so. It is common to have significant swelling because of the surgery and the wounds can leak for a few days afterwards as the swelling reduces.
After 3 days the bulky bandage can be removed / after one week the dressings can be removed. If you have any sutures that need removing we will tell you. In general, the sling is worn for around 3 weeks, full range of movement is achieved by around 3 months and you can return to sporting activities around six months. If you choose to return to sporting activities sooner your risk of dislocation is slightly higher.
Complications
Common risks include bleeding, infection, pain and stiffness in the shoulder.
Specific risks with this operation are
Failure to prevent dislocation / recurrence (5-10%)
Nerve injury (<1%)
Further surgery required if re-dislocation
Results
90-95% of those undergoing stabilisation do not have any further dislocations. That said around 15% of patients find they do not trust their shoulder as they used to before it dislocated. Most of these will require no further surgery but some may go on to require an open procedure to enable them to work or return to sports.
Total Shoulder Replacement
Introduction
Anatomic Total Shoulder Replacement (A-TSR) is an operation to treat arthritis of the shoulder. For this operation to work and last for a number of years, the tendons (rotator cuff) around the shoulder must be intact and functioning. For this reason, not everyone with shoulder arthritis can have an A-TSR. If your rotator cuff is not functioning properly & you require a shoulder replacement, you will more than likely be offered a reverse polarity total shoulder replacement (rp-TSR).
The Operation
You will normally be admitted on the day of surgery unless you have any specific medical complaints that require prior admission. You will be seen by a nurse, a doctor and maybe a physiotherapy before you go to theatre for your surgery; you will have opportunity to ask any further questions prior to the operation. The anaesthetic time and operation lasts around 2-3 hours. You will be asleep under general anaesthetic and may also have a nerve block to control your pain after the surgery. During the operation we replace the diseased and painful parts of your shoulder joint (the ball with metal and the socket with a hard plastic).
After Surgery
On the morning following surgery you will have an x-ray of the shoulder to check for any fractures we may have caused but not noticed and that the new shoulder is in the correct position. During the x-ray your arm may be moved; do not worry these are the views we need to get to ensure the images are accurate. We will look at the x-rays before your discharge. You may require blood tests after your surgery, though this is not always the case. The physiotherapists will arrange followup and tell you what you can and can’t do with your shoulder. Most people will go home on the first day following surgery but we will never discharge you until you’re safe.
Complications
The general complications include bleeding, infection, stiffness and ongoing pain.
Specific complications with this procedure include:
dislocation of or fracture around the new shoulder prosthesis
nerve injury (2% but most recover fully)
loosening of the prosthesis requiring further surgery
Results
Overall between 85-90% of individuals have a good or excellent outcome one year following surgery. Pain can improve up to two years following surgery but you still may have a small amount of pain permanently. Range of movement is a little unpredictable following surgery but it is unlikely to be worse than your current range of movement. We try to perform outcome scores at 3 months, 6 months, 1 year and 2 years following your surgery; this is to let us know how well you’ve done in relation to regional and national averages.
Follow up
We will normally see you in a follow up clinic at 2 weeks to check for early complications and then at frequent intervals with x-rays to check the shoulder continues to function well.
National Joint Registry (NJR)
The NJR records data about your shoulder replacement to track the implant and see how well it performs, to enable us to continue to improve the level of care we provide. We also ask you to provide certain personal details (with your consent) to match your implant to you and follow it through in the long-term. To see more about how the NJR functions, click here.
For more information from the NJR about Shoulder Replacement click here.
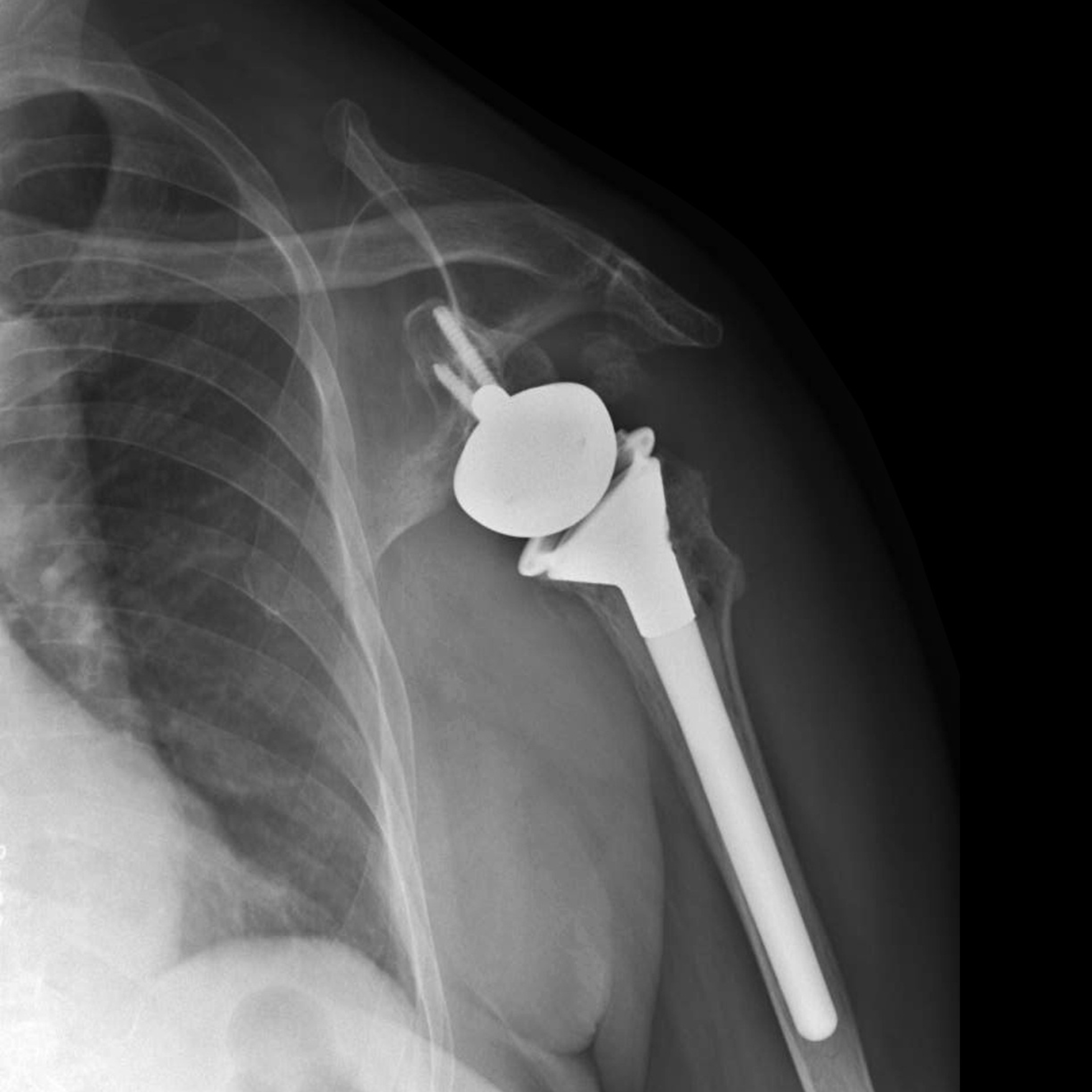
Reverse Polarity Total Shoulder Replacement
Introduction
Reverse polarity total shoulder replacement (rp-TSR) is an operation to treat arthritis of the shoulder with pain, associated with massive irreparable tears in the tendons (rotator cuff) around the shoulder. It is reserved as a last resort as though in the majority of cases they function well, the complications are serious if encountered. For this operation to work the deltoid muscle must be functioning as it alone allows the new shoulder replacement to function. In addition, because there are limited options after reverse shoulder replacement we tend not to offer this surgery in younger patients (<65 years) but these rules are flexible to some extent. If you are young with a massive irreparable rotator cuff tear, there are other options available to you.
The Operation
You will normally be admitted on the day of surgery unless you have any specific medical complaints that require prior admission. You will be seen by a nurse, a doctor and maybe a physiotherapy before you go to theatre for your surgery; you will have opportunity to ask any further questions prior to the operation. The anaesthetic time and operation lasts around 2-3 hours. You will be asleep under general anaesthetic and may also have a nerve block to control your pain after the surgery.
During the operation we replace the diseased and painful parts of your shoulder (ball-and-socket) joint. It is called REVERSE shoulder replacement because we exchange the ball for a socket made of hard plastic, and the socket for a metal ball. This serves to position the shoulder joint slightly lower than it was before allowing the deltoid muscle to elevate the arm up towards shoulder height without pain.
After Surgery
On the morning following surgery you will have an x-ray of the shoulder to check for any fractures we may have caused but not noticed and that the new shoulder is in the correct position. During the x-ray your arm may be moved; do not worry these are the views we need to get to ensure the images are accurate. We will look at the x-rays before your discharge. You may require blood tests after your surgery, though this is not always the case. The physiotherapists will arrange followup and tell you what you can and can’t do with your shoulder. Most people will go home on the first day following surgery but we will never discharge you until you’re safe.
Complications
The general complications include bleeding, infection, stiffness and ongoing pain.
Specific complications with this procedure include:
dislocation of or fracture around the new shoulder prosthesis
nerve injury (2% but most recover fully)
loosening of the prosthesis requiring further surgery
Results
There are no long-term outcome studies looking at rp-TSR, though early results are promising. Especially in comparison to hemiarthroplasty (half joint replacement of the ball only) for either rotator cuff disease or unreconstructable fractures of the shoulder. We try to perform outcome scores at 3 months, 6 months, 1 year and 2 years following your surgery; this is to let us know how well you’ve done in relation to regional and national averages, and to generate results to publish internationally.
Follow up
We will normally see you in a follow up clinic at 2 weeks to check for early complications and then at frequent intervals with x-rays to check the shoulder continues to function well.
National Joint Registry (NJR)
The NJR records data about your reverse shoulder replacement to track the implant and see how well it performs, to enable us to continue to improve the level of care we provide. We also ask you to provide certain personal details (with your consent) to match your implant to you and follow it through in the long-term. To see more about how the NJR functions, click here.
For more information from the NJR about Shoulder Replacement click here.